Oaklyn's Story, 27 Weeks

Miracle Mum, Amy had to make an impossible decision and suffered through immense trauma both physically and psychologically. She shares the story of bringing tiny Oaklyn into the world and how they both fought for their life.
"I found out I was pregnant on Jan 26th. We already had five children (four via c-section) and weren’t planning on any more, but life had other plans. We quickly became excited about welcoming our 6th baby. I began spotting at five weeks which I automatically assumed may be a miscarriage. The hospital ran bloods and my hCG levels were normal. I sighed with relief but worried what was causing it. They sent me to the women’s hospital for an ultrasound as I previously had an ectopic pregnancy (2nd pregnancy) and wanted to rule that out. We went to the hospital and they called my private obstetrician. She did an ultrasound and showed me a tiny flutter but I could see she was concerned. She said to me I can see a baby BUT it looks to be in your c section scar. She told me that if it was it would need to be a termination. She spoke to another doctor and she said it was difficult to tell if it was or wasn’t in or on the scar. Due to the baby being implanted so low I was either going to miscarry or the pregnancy would continue. She gave me a 50\50 chance. As the days went on the bleeding became heavy, however I had no pain. Two weeks later we returned for a follow up scan; due to the bleeding I had somewhat processed that we had lost our baby. My husband was working offshore on the oil rigs and I told him not to fly back early as I had a strong feeling the baby wouldn’t be there. On the ultrasound there was a baby, measurements exactly where they should be and a strong heartbeat. Still very low but seemed to be continuing. I asked about the bleeding and my obstetrician said its location would make it more of an issue.
At 10 weeks I had my first formal obstetricianappointment. She looked at the ultrasound for some time and said the pregnancy appeared highly vascular. I had no idea what this meant. She sent me for a scan with the maternal foetal specialist for 13 weeks. This scan revealed that I had Placenta Accreta, but not just accreta. Percreta. My heart sank. I asked him what this meant for my baby and he said he would strongly urge us to consider terminating. My heart was broken and I couldn’t comprehend what was going on. After countless tears and pros and cons my husband and I decided to continue the pregnancy. At 13 weeks we found out we were having a little girl. From then on I had ultrasounds fortnightly until 18 weeks. I started spotting and was told that if any bleeding occurred I needed to go to hospital ASAP. My obstetrician scanned and she said ‘Amy, this pregnancy is becoming life threatening for you’. I have never seen a percreta like this. She then strongly suggested termination, which I declined . My mother was with me and begged me to reconsider due to our other children. In this moment I was torn; do I terminate now for my five children or do I continue for our daughter? My heart and head were very divided, and I just didn’t know what was right. I did a lot of soul searching and I knew in my heart I just couldn’t bring myself to terminate. This decision wasn’t supported by my family.
The next morning we had a formal scan and MRI as I was then admitted to the hospital. The mat-foetal specialist told us that this was the worst percreta he had ever seen and it was highly unlikely we would make it to viability at 23 weeks without a major bleed. He also explained if I did have a bleed it would be life threatening and within 8-10 minutes my body wouldn’t be able to survive. This meant I had to stay in hospital for the duration of the pregnancy. Being away from my kids was hard, my husband was working full time along with being a mum and a dad. We relied on our family and friends to help with our kids. I saw the kids one weekend day a week due to the hospital being 60mins away from our home. Every day I counted down to viability and the chance our baby could live; I almost forgot that my life was also in the balance. It became about keeping her safe and giving her the best chance. The days passed and we got to 23, 24, 25 weeks. My heart was so full and I even began discussing the option of going beyond 34 weeks which was the planned delivery duration of an accreta pregnancy. I had been stable and had no bleeds in weeks, so my obstetrician decided as long as my husband was home with me, I could go home. I packed my things and was so excited!
Two days later I was having dinner and felt the need to go to the toilet. As I sat down all I saw was blood, everywhere. I knew that time was critical. My husband froze as I yelled out I needed help. I rang the ambulance and they were here almost immediately. I began to get dizzy and they decided to transport me to the Women’s Hospital with lights and sirens in the hope we could beat the clock. We made it to the hospital and the room filled with doctors. I hadn’t felt my baby move for hours at this point and questioned if she was even alive. Thankfully, they found her heartbeat, and I could breathe. The doctor said if the bleeding didn’t stop then we would be delivering that evening. But it slowed. Such a miracle! Two days later at 26+6 I was able to go back to the ward at the hospital. In the early hours of that morning I began getting pain in my left side. At first I thought nothing of it but as the hours passed it became intense. I called the nurse and she was very concerned knowing the history and risks, they decided to send me back to labour and delivery. Once I was there, I called my husband and he came in. My obstetrician came in and told me it was time to have our baby. Another doctor and the Medical Director came in and discussed the plan with me. I knew things were bad when they came in and took over my care. They organised an urgent MRI to measure where the percreta was and the damage. I remember being in the machine and I could see the whole room with doctors looking and pointing at the screen. This was the first time I questioned if I had made the right decision. I was terrified.
I went back to my room and the anaesthetist came in to put in an operating IV. I didn’t have a lot of information at this point and nor did he. The two doctors then returned and told me that things were not looking good, the pain I had been feeling was the percreta taking over my left ureta. It had also consumed my cervix, bladder, invaded my bowel and my iliac artery. I could see the fear as he spoke and that made me realise this wasn’t going to go how I had it planned in my head. They then told me I couldn’t deliver at the women’s hospital and would need to deliver at the trauma hospital… which wasn’t a maternity hospital and they had never delivered a baby. So, this meant all equipment and teams were going to go over and work with each specialist team on their organ.
I was transferred and taken to my room. I was overwhelmed with the news and just didn’t know how to digest it. The teams started coming in one after another telling us the risks and dangers. The vascular team told me it was highly likely I may not walk or regain complete function in my legs due to vascular damage, skin infections and feeling, a colostomy bag due to bowel damage, long term bladder issues, hysterectomy etc. Next was the neonatal team, then it all hit me how early our baby was going to be and what that meant for her. 13 weeks before she should be coming into the world. What was I thinking? Why did I do this? I started crying because it just got on top of me. It was all out of my control and I just had to stay strong. I was given a 20% chance of survival.
My surgery was the next day at lunch time. I cried all morning while I was in the shower and toilet breaks. How in the world could I leave my children? I may never even meet my baby. I refused to be taken down to theatre and went into a panic. My husband and mother were trying to keep me calm but I had been so collected until this point. Eventually I held my husband’s hand and said I will see you soon. My best friend sent me a text - you will get through this, it is not over. I sat in the prep area and couldn’t hear anyone; people were talking and asking me to sign documents and it was all a complete blur. In theatre I can remember seeing so many people, that it was overwhelming. Later I found out we had 32 staff in theatre. I begged for them to put me out but my oxygen was too low and needed to be stabilised. Finally, I was out.
Nine hours and 46 minutes later my surgery was finished. My heart stopped three times during surgery. Our beautiful daughter Oaklyn Hope was born two hours into surgery weighing a tiny 1kg. Due to her being under the effects of a general anaesthetic for so long, she was born lifeless and intubated immediately. She was then whisked off to the Women’s Hospital via the neonatal intensive transport team. I woke up at midnight in ICU with a tube in my throat. I was extubated 30 minutes later. I could feel my legs thank goodness. I had a scar from my chest down to my previous C-section and hiatus sheeths for pain relief. I couldn’t move my body, I was numb. I couldn’t feel any pain but I knew my body had just endured a serious event. The nurse spoke to me asking how I felt, but all I wanted to know was information on my baby. She didn’t know. Eventually the hospital sent a photo of our daughter’s face and all the information about her. I was relieved that she was alive. I spent five days in ICU and begged them every day to let me be transferred to the special care unit at the Women’s Hospital. But I wasn’t stable enough.
Finally, I was able to go back there and be managed. The paramedics asked if I had met my baby, but I told them I wasn’t well enough. They surprised me by taking me via the NICU to meet my tiny baby. It was surreal; I was excited but scared for what I was about to see. Then - there was my tiny baby under a blue light in a humidicrib. Her little feet flickering like she would have inside of me. I couldn’t believe she was so fully formed, just like a tiny version of a newborn. I was in love, but I was scared. I was scared I would lose her and I knew the journey was just starting.
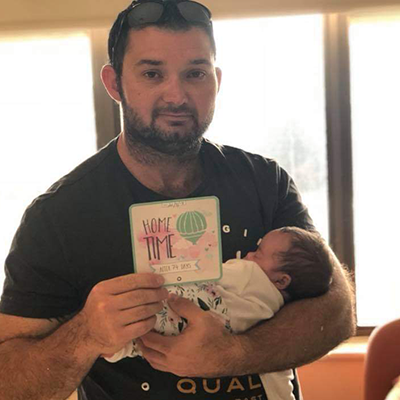
The next few days I visited Oaklyn as much as I could from critical care. I couldn’t walk as yet and I was starting to feel what pain really was. I developed an infection that became serious and was readmitted to ICU. Once that was managed, I came back to critical care. It was 29 days from my surgery to finally going home. But going home wasn’t as easy as I had thought. Seeing my kids was absolutely amazing, but I left without a baby. Our kids were confused as to why she wasn’t home and I didn’t speak of Oaklyn in fear they would endure the possibility of losing a sister. I was so protective of their and my feelings, that I didn’t want to connect with Oaklyn. I was on high alert and had been for so long I didn’t know how to stop it. There were days I couldn’t go to the NICU because I couldn’t bring myself to move. I was still recovering physically and emotionally from a major trauma. I was lucky to have the psych team support and was given medications to assist in keeping some stability in my mind and to help me sleep. I pumped every two hours ensuring she was getting my milk as the doctors told me how important it was for a prem to have breast milk. My mental health deteriorated and at times I cried and wished I hadn’t done it. I couldn’t comprehend what had happened, I just wanted to erase it. Oaklyn spent 76 days in the NICU. She had a relatively good run although developed NEC which is a bowel infection. They told us at the time that it’s the leading cause of premature babies’ deaths and we were terrified. But she beat it. Eventually we brought her home and it was so amazing having both of us together with our family.
I didn’t realise how a hysterectomy would affect me, but it has. We weren’t planning on more children but once the chance was gone it was processing a sense of loss. A sense of losing that part of me that made me a woman. It took me some time to come to terms with the fact that my body wasn’t the same. I look at the incision every day and remember what had happened. As time goes on it’s slowly getting easier. Oaklyn is 16 months old and has challenges, but overall her outcome was pretty amazing, considering.
My journey is one of the ones that’s semi positive: we both made it. It’s a challenge making huge decisions for two people and potentially your entire family. But we survived."

Want to share your story too? We welcome every Miracle family story, no matter what stage of the journey you're at.
We encourage those wishing to share their story to submit it below:




